This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.

Treating haemorrhoids with radiofrequency
What are haemorrhoids?
Haemorrhoids, or piles, are natural cushions of tissue and blood vessels in the anus and lower rectum. They help with stool control by getting smaller to allow waste to pass through. Everyone has these cushions, and we usually don’t give them a second thought, but occasionally they can become swollen or inflamed. Most of the time, when we’re talking about “haemorrhoids” or “piles”, that’s the condition we mean.
Haemorrhoids are very common—around half of us will experience them at some point in our lives. Sometimes, they go away on their own, or with a few minor lifestyle changes; other times, they require medical attention.
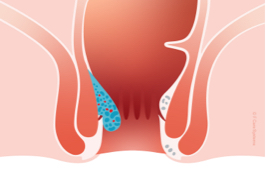
Haemorrhoids can develop internally (inside the rectum) or externally (down the anus).
We grade internal haemorrhoids by size and severity:
- Grade 1 haemorrhoids are the smallest, and they don’t prolapse (= protrude from the anus).
- Grade 2 haemorrhoids prolapse during a bowel movement, but then return to their original position.
- Grade 3 haemorrhoids prolapse during a bowel movement and have to be repositioned manually (pushed back inside).
- Grade 4 haemorrhoids are the largest; they are always prolapsed (they can’t be repositioned), and they typically have additional complications, such as inflammation.


What causes haemorrhoids?
Haemorrhoids result from increased anal or abdominal pressure, which causes the tiny veins inside the piles to swell (like varicose veins). A lot of things can create this additional pressure, especially:
- Sitting on the toilet for long periods
- Straining when using the toilet (constipation)
- Being overweight
- Doing a lot of heavy lifting
- Pregnancy
Anyone can develop haemorrhoids, though they’re more common in older people and tend to run in families. Diet can be a major factor as well, since constipation and haemorrhoids are frequently linked. Many people know that a lack of dietary fibre can lead to constipation, but another, often overlooked cause is dehydration: when the body isn’t getting enough water, the large intestine will absorb more water from food waste, which means harder stools that are more difficult to pass.
How do I know if I have haemorrhoids?
Not everyone who develops haemorrhoids has symptoms, and not everyone who has symptoms gets them all the time. Possible symptoms may include:
- Bright red blood on the toilet paper, in your stool, or in the bowl
- Rectal itching or pain, especially when sitting
- Pressure or urgency (feeling like you still need to use the toilet after going)
- Mucus in your underwear or on the toilet paper after wiping your bottom
- Lumps around your anus that feel sore or tender
Some people find haemorrhoid symptoms embarrassing to talk about, but it’s important to seek medical care if they don’t go away, to make sure they’re not a sign of anything more serious.
What can I do about my haemorrhoids?
Many people develop haemorrhoids due to constipation, so staying “regular” is one of the most important things you can do to manage them.
To prevent constipation:
- Eat more fibre (wholemeal bread, wholegrains, pulses, fresh or dried fruits, vegetables)
- Drink plenty of water every day
- Exercise regularly
- Cut down on caffeine and alcohol
- Don’t sit on the toilet for long periods
- Empty your bowels when you need to—don’t hold it for too long!
Managing your weight can also help with piles by reducing the pressure on your abdomen.
Warm sitz baths or ice packs can alleviate rectal pain and swelling, and there are a variety of creams and ointments on the market as well. Don’t take anti-coagulants if you have bleeding haemorrhoids. Make sure to keep your bottom clean and dry, and avoid wiping too hard.
Treating haemorrhoids with Rafaelo®
Patients with Grade 2, Grade 3 and some Grade 4 internal haemorrhoids may benefit from Rafaelo®, a system developed in 2016 for treating haemorrhoids using high-frequency radio waves.
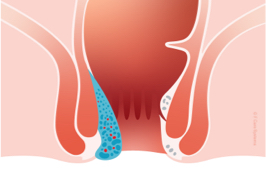
Rafaelo® stands for RadioFrequency ablation (= removal) of hAEmorrhoids under LOcal anaesthesia. After injecting a small amount of anaesthetic, your doctor will insert a very thin probe into the haemorrhoid and apply targeted radiofrequency energy.
The heat from the radio waves causes the pile to shrivel up and scar, but without damaging the healthy tissue around it. The whole procedure takes just a few minutes, and most people can return to their usual activities the next day. Your doctor may prescribe analgesics (painkillers) in case you experience any discomfort in the following few days, but many patients have no further symptoms at all.
Advantages of Rafaelo®
- Quick outpatient procedure (approx. 15 minutes)
- Can be performed under local anaesthesia
- Minimally invasive (no surgical incisions)
- Return to work/regular activities almost immediately
- Little to no pain during or after treatment
- Safe and effective treatment
Where can I find treatment?
Alternative treatments
Sphera
Rafaelo® is intended to treat internal haemorrhoids of Grades 2, 3, and early 4. For smaller haemorrhoids (Grades 1 and 2), your doctor may instead elect to use a Sphera ball probe. The Sphera uses the same basic radiofrequency ablation technology, but only on the outside of the pile (unlike the HPR45i needle probe in Rafaelo®, which is also inserted into the pile).
Rubber band ligation
Another safe and effective non-surgical option for smaller internal haemorrhoids (Grades 1 and 2) is rubber-band ligation, for example using the Pilex ligator. In rubber-band ligation (or RBL), the doctor uses suction to draw the haemorrhoid into the nozzle of the Pilex tool, and then quickly wraps a very small rubber band around the base of the pile. The rubber band cuts off the blood supply to the pile, causing it to wither and drop off over time (usually within a week). There are no nerve endings in piles themselves, so RBL is naturally painless without anaesthesia, though your doctor may prescribe some painkillers in case you feel any discomfort in the general area afterward.

